Opioid Epidemic: Back in the spotlight as overdose concerns rise, COVID-19 deaths wane
November 14-20, 2022
By Wesley Brown
Before the COVID-19 pandemic descended upon the nation, Arkansas and several other poor, rural southern states were dealing with an epidemic that at the time was described by the U.S. Center for Disease, Control and Prevention (CDC) as a national crisis.
In fact, shortly after the pandemic took hold in September 2020, three doctors within the National Institute for Occupational Safety and Health (NIOSH) said the U.S. was already facing a public health crisis with the evolving and worsening drug overdose epidemic. NIOSH is the federal agency responsible for conducting research and making recommendations for preventing work-related injury and illness. It is part of the CDC and housed within the U.S. Department of Health and Human Services.
According to NIOSH doctors Drs. Jamie Osborne, L. Casey Chosewood and John How, the alarming rates of opioid-related overdose deaths ahead and at the beginning of the pandemic was cause for national concern. For example, 46,802 deaths in 2018 were attributed to opioids, which accounted for 69% of all drug overdose deaths. In the following year before the pandemic, an estimated 50,828 Americans died of opioid overdose in 2019 — 70% of the total estimated drug overdose deaths last year.
“As COVID-19 has swept the nation and globe, the virus and its implications have had particularly harmful impacts on individuals struggling with opioid misuse, opioid use disorder (OUD), and overdose. The co-occurring COVID-19 pandemic and opioid overdose epidemic have created what some have called ‘the perfect storm for folks who are substance dependent,’” said the NIOSH doctors. “The mortality rate for patients with a substance use disorder is predicted to be significantly higher than the general population, indicating that ‘epidemics don’t smolder during pandemics — they ignite.’”
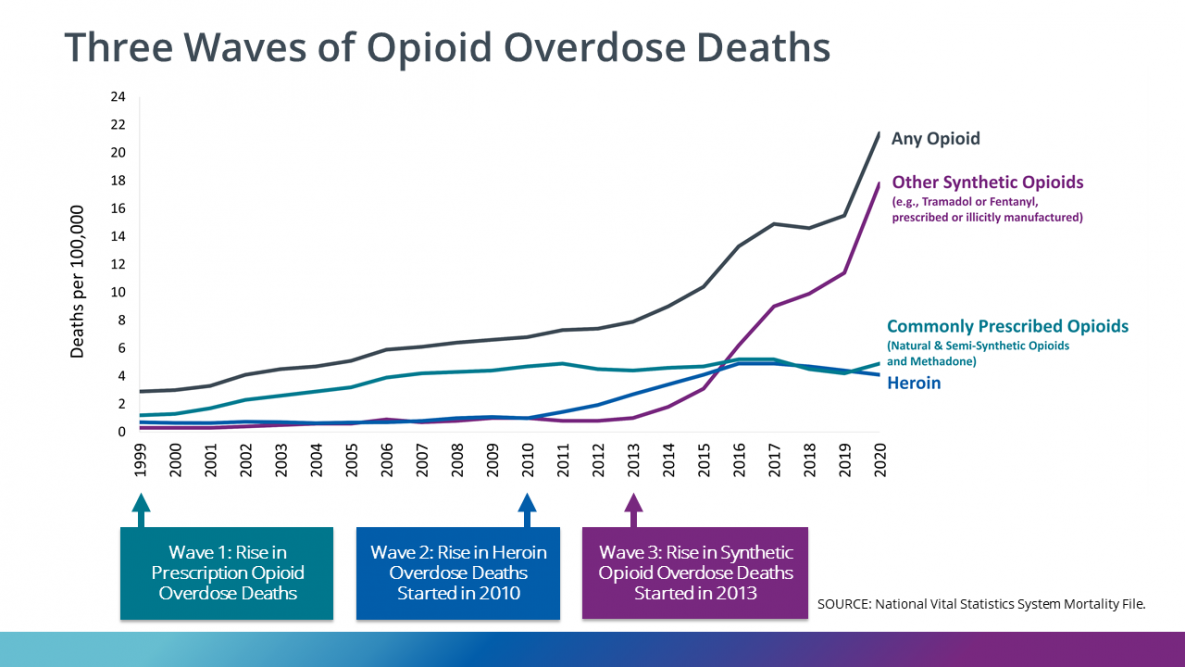
Nationally, the death rate from drug overdose in the United States from the so-called opioid epidemic has risen steadily since 1999 and hit a record high in 2020. That year there were around 28 overdose deaths per 100,000 population, compared to a rate of six per 100,000 population in 1999. Most of these overdose deaths involve opioids such as prescription opioids, heroin, or illegally manufactured synthetic opioids like fentanyl.
This sharp rise in opioid abuse and overdose deaths in the United States is known as the opioid epidemic. Although the government declared the opioid epidemic a public health emergency in 2017, the epidemic has only worsened in recent years, intensifying under the shadow of the COVID-19 pandemic. The opioid epidemic has come in three distinct waves: the first was a rise in overdose deaths from prescription opioids; the second, a sharp increase in overdose deaths involving heroin; and the third, and most deadly, a substantial increase in deaths involving synthetic opioids, namely fentanyl.
ARKANSAS’ OPIOID CRISIS
Before the COVID-19 health crisis began, CDC data shows that Arkansas was one of the 50 states that was hardest hit by the opioid epidemic. In fact, a 2017 CDC report showed that all but nine of Arkansas’ 75 counties had overall opioid prescribing rates higher than the national average of 66.5 prescriptions per 100 people. As a state, Arkansas has an opioid prescription rate of 114.6 per 100, second only to Alabama’s 2016 average of 121 per 100 people.
During a Joint Interim Committee on Public Health at the State Capitol during the 2017 legislative session, then-Arkansas Department Health (ADH) Director Nate Smith gave a report to lawmakers that enough opioids are now being sold in Arkansas for every man, woman and child to take 80 pills each over the course of a year.
After a steady increase in the overall national opioid dispensing rate starting in 2006, the total number of prescriptions dispensed peaked in 2012 at more than 255 million and a dispensing rate of 81.3 prescriptions per 100 persons. The overall national opioid dispensing rate declined from 2012 to 2020, just as the COVID-19 pandemic began.
According to the most recent CDC data from 2020, the dispensing rate has fallen to the lowest in 15 years. At the end of 2020, the national dispensing rate stood at 43.3 prescriptions per 100 persons for a total of more than 142 million opioid prescriptions. Despite those improvements, CDC officials said dispensing rates continued to remain very high in certain areas across the country, including Arkansas.
“While the overall opioid dispensing rate in 2020 was 43.3 prescriptions per 100 people, some counties had rates that were nine times higher than that,” the CDC warns.
In Arkansas, the dispensing rate in 2020 was second in the nation at 75.8%, trailing only Alabama at 80.4%. Still, Arkansas’ dispensing is well above the national average at 43.3 prescriptions per 100 persons. Of the 75 counties in Arkansas, Craighead County has the highest dispensing rate at a whopping 164%, followed by Pulaski and Baxter counties at 141.7% and 136.7% at the end of 2020, CDC data reports.
Other Arkansas counties exceeding a 100% dispensing rate included Garland (112.9%), Independence (132.5%), Sebastian (121.5%) and Union (113.6%). Nationally, in 3.6% of U.S. counties, enough opioid prescriptions were dispensed for every person to have one at the end of 2020.
According to CDC data, the six states with the highest dispensing rates are all southern, rural states that have also seen a spike in the number of opioid-related overdoses. They include Arkansas, Alabama, Kentucky, Louisiana, Mississippi and Tennessee.
CDC data shows that more than 932,000 people have died since 1999 from a drug overdose. In 2020, 91,799 drug overdose deaths occurred in the United States. The age-adjusted rate of overdose deaths increased by 31% from 2019 (21.6 per 100,000) to 2020 (28.3 per 100,000).
Opioids — mainly synthetic opioids such as fentanyl — are currently the main driver of drug overdose deaths, causing 82.3% of opioid-involved overdose deaths involving synthetic opioids. Opioids were involved in 68,630 overdose deaths in 2020, which is 74.8% of all drug overdose deaths.
Arkansas was among the top ten states with the highest rate of overdose death increases in 2020, just as the COVID-19 pandemic peaked across the U.S., CDC data shows. The age-adjusted rate of overdose deaths increased by 41.5% from 2019. Mississippi (55.1%), West Virginia (54.2%), South Carolina (53.7%), Louisiana (51.4%) and Kentucky (50.9%) were the states with the highest rate of overdose death increases amid the ongoing pandemic.
CDC REVERSES RECOMMENDATIONS ON PRESCRIBING OPIOIDS
In response to more recent concerns about opioid use and the effect pain has on the lives of millions of Americans every day, the CDC released updated and expanded recommendations for clinicians providing care for adult outpatients with short- and long-term pain. These recommendations, published in the CDC Clinical Practice Guideline for Prescribing Opioids for Pain, will help clinicians work with their patients to ensure the safest and most effective pain care is provided. The publication updates and replaces the CDC Guideline for Prescribing Opioids for Chronic Pain released in 2016.
“Patients with pain should receive compassionate, safe and effective pain care. We want clinicians and patients to have the information they need to weigh the benefits of different approaches to pain care, with the goal of helping people reduce their pain and improve their quality of life,” said Christopher M. Jones, a pharmacist and acting director of CDC’s National Center for Injury Prevention and Control.
The 2022 Clinical Practice Guideline addresses the following areas: 1) determining whether to initiate opioids for pain, 2) selecting opioids and determining opioid dosages, 3) deciding duration of initial opioid prescription and conducting follow-up, and 4) assessing risk and addressing potential harms of opioid use. The Clinical Practice Guideline supports the primary prevention pillar of the HHS Overdose Prevention Strategy — supporting the development and promotion of evidence-based treatments to manage pain effectively.
The guideline is a clinical tool to improve communication between clinicians and patients and empower them to make informed decisions about safe and effective pain care. The recommendations are voluntary and provide flexibility to clinicians and patients to support individualized, patient-centered care. They should not be used as an inflexible, one-size-fits-all policy or law or applied as a rigid standard of care or to replace clinical judgment about personalized treatment.
CDC said it followed a rigorous scientific process using the best available evidence and expert consultation to develop the 2022 Clinical Practice Guideline. An independent federal advisory committee, four peer reviewers, and members of the public reviewed the draft updated guideline, and CDC revised it in response to this feedback to foster a collaborative and transparent process. CDC also engaged with patients with pain, caregivers and clinicians to gain insights and gather feedback from people directly impacted by the guideline. The expanded guideline aims to ensure equitable access to effective, informed, individualized and safe pain care.
“The science on pain care has advanced over the past six years,” said Dr. Debbie Dowell, chief clinical research officer for CDC’s Division of Overdose Prevention. “During this time, CDC has also learned more from people living with pain, their caregivers and their clinicians. We’ve been able to improve and expand our recommendations by incorporating new data with a better understanding of people’s lived experiences and the challenges they face when managing pain and pain care.”
CDC said it will continue to work to improve patient safety and outcomes by equipping healthcare professionals and patients with data, tools, and guidance they need to make informed treatment decisions. The 2022 Clinical Practice Guideline supports patients and clinicians in making informed, individualized decisions about safe and effective pain care.
Photo Captions"
1. Opioid epidemic back in the spotlight as overdose concerns rise, COVID-19 deaths wane
2. The Centers for Disease Control and Prevention (CDC) on Nov. 3 released updated and expanded recommendations for clinicians providing pain care for adult outpatients with short- and long-term pain. These clinical recommendations, published in the “CDC Clinical Practice Guideline for Prescribing Opioids for Pain,” will help clinicians work with their patients to ensure the safest and most effective pain care is provided.
3. From 1999–2020, more than 564,000 people died from an overdose involving any opioid, including prescription and illicit opioids. The first wave began with increased prescribing of opioids in the 1990s, with overdose deaths involving prescription opioids. The second wave began in 2010, with rapid increases in overdose deaths involving heroin. The third wave began in 2013, with significant increases in overdose deaths involving synthetic opioids, particularly those involving illicitly manufactured fentanyl.
4. In 2020, heroin-involved overdose death rates decreased nearly 7% from 2019 to 2020. The number of heroin-involved overdose deaths was nearly seven times higher in 2020 than in 1999.