Arkansas awarded nearly $92 million in federal funding for COVID-19 testing
May 25-31, 2020
By Daily Record Staff
On the same that Arkansas and several other states began their board reopening plans, the U.S. Department of Health and Human Services (HHS) announced that Arkansas will receive $91.3 million to provide critical support to “develop, purchase, administer, process, and analyze COVID-19 tests” and other related activities.
Under the second round of stimulus funding approved by Congress under the Paycheck Protection Program and Health Care Enhancement Act on April 23, HHS said the Centers for Disease Control and Prevention (CDC) will provide $10.25 billion to states, territories, and local jurisdictions through CDC’s existing Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases (ELC) cooperative agreement.
The Indian Health Service (IHS) will provide another $750 million to IHS, tribal, and urban Indian Health programs to expand testing capacity and testing-related activities. This funding is part of the Trump Administration’s broader effort to ensure that states, territories, and tribes have the resources necessary to meet their testing goals as they begin to reopen.
“This funding secured by President Trump for state, tribal, and local public health activities is a historic investment in America’s ability to track and control the spread of the virus, which is essential to a safe reopening,” said HHS Secretary Alex Azar. “For the sake of all Americans’ health and well-being, we must help Americans get safely back to work and school, and that requires continued expansion of testing, surveillance, and contact tracing. The Trump Administration stands ready to support and guide states in their life-saving work to combat the virus and reopen our country.”
Added CDC Director Dr. Robert Redfield: “As the Nation cautiously begins the phased approach to reopening, this considerable investment in expanding both testing and contact tracing capacity for states, localities, territories and tribal communities is essential,”
“Readily accessible testing is a critical component of a four-pronged public health strategy – including rigorous contact tracing, isolation of confirmed cases, and quarantine,” continued Redfield. As communities move toward a blended mitigation and containment strategy, I encourage all Americans to continue to embrace powerful public health measures – social distancing, hand washing and face coverings. We are not defenseless in the battle against this pandemic.”
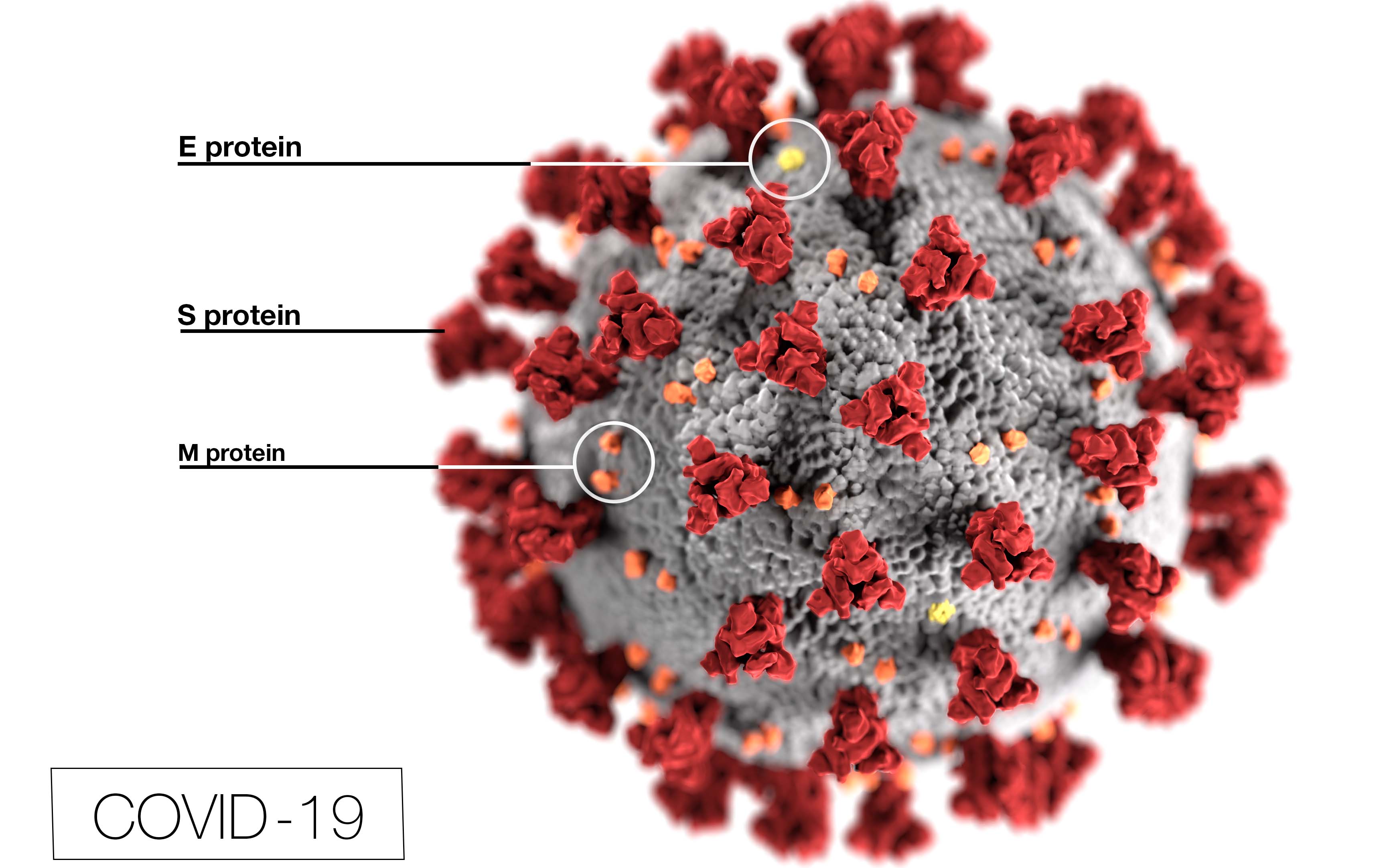
Since the first positive COVID-19 case in Arkansas in early March, Congress has approved four emergency relief bills to deal with the health and economic implementations from the virus that causes COVID-19, known as SARS-CoV-2.
The first emergency bill was the $8.3 billion Coronavirus Preparedness and Response Supplemental Appropriations Act that was approved on March 6. That bill provided funding for emergency health and medical supplies and equipment and other needs through several federal agencies, including the Food and Drug Administration, the Centers for Disease Control and Prevention, and the National Institutes of Health. The bill also included temporary waivers or application modifications of certain Medicare requirements associated with telehealth services.
The second emergency bill, known as the Families First Coronavirus Response Act, appropriated nearly $4 billion in tax credits and other measures focused on free coronavirus testing, new paid leave requirements, enhanced food stamp and unemployment benefits and increased federal Medicaid funding.
The third and most familiar bill, known as the CARES Act or Coronavirus Aid, Relief, and Economic Security Act, represented a sweeping $2.2 billion investment in state and local government, major industries, small and midsize businesses, public health, and disaster relief programs.
That new law included the now famous Paycheck Protection Program (PPP) administered by the U.S. Small Business Administrative provided forgivable loans up to $10 million to small businesses left financially distressed by the coronavirus COVID-19 pandemic. Those loans, however, quickly ran out of funds in only two weeks after by a national network for more than 100 banks and credit unions began accepting applications on April 3.
In Arkansas, more than 100 Arkansas banks and lenders processed 21,754 PPP loans totaling more than $2.72 billion, according to the SBA’s District Office in Little Rock. Under CARES Acts rules, the loans were provided to small businesses without collateral requirements, personal guarantees, SBA fees, or credit elsewhere tests. Supposedly, those eligible for the program include small businesses, certain non-profits, veterans’ organizations, self-employed individuals, independent contractors, and other businesses with fewer than 500 employees.
However, those programs ran out of funds in just two weeks after several small business groups claimed that the nation’s four largest banks and other large SBA-approved lenders in the PPP program rigged the loan process to benefit their bottom line to the tune of nearly $6 billion in commission and fees. According to the federal complaints, instead of a “first-come, first-served” application process after the PPP program was launched on April 3, many banks processed the biggest loan amounts first because of profitable origination fees. That method left more than 90% of the true small businesses still in the SBA’s queue once funds were depleted.
As the criticism of the program fund grew louder, Congress approved the Paycheck Protection Program and Health Care Enhancement Act. That new $484 billion law, signed into law on April 24, increases PPP loans by $310 billion and provided new funding for hospitals and testing for COVID-19.
For its part, Arkansas’ share of the $11 billion in COVID-19 testing funding will included $78.2 million for COVID-19 testing. That new round of funding will be added to the more than $13 million appropriated to the state from the first three COVID-19 emergency relief bills.
Under the new act, governors and health departments in all 50 states must provide feedback to HHS on the number of tests needed, monthly estimates of laboratory and testing capacity in the workforce, and a description of how resources for testing are being used to mitigate new COVID-19 cases. States must also use the funding they receive to meet the testing goals laid out in their COVID-19 testing plans, including purchasing testing supplies and PPP when necessary.
Despite nearly $3 trillion in coronavirus related funding already approved by Congress, along with an additional $2.3 billion in liquidity and credit from the Federal Reserve, many U.S. lawmakers and trade groups are pushing for additional support as the search for a COVID-19 vaccine continues.
On May 15, the U.S. House of Representatives approved a larger $3 trillion bill aimed at providing relief and support to those impacted by the coronavirus pandemic. That bill, known as the Health and Economic Recovery Omnibus Emergency Solutions Act, or the HEROES Act, surpasses the first CARES Act stimulus package by nearly $800 million. Although it was approved in the House by a largely bipartisan vote of 208 to 199, it has stalled in the GOP-controlled Senate.
Meanwhile, the nursing home industry is requesting that any next round of COVID-19 emergency relief includes funding to cover the cost of testing residents and staff at assisted living and other long-term care facilities.
According to the American Health Care Association and National Center of Assisted Living (AHCA/NCAL), the cost of ongoing COVID testing of nursing home residents and staff is unsustainable without additional funding and support from federal and state governments. Even the CDC’s recent recommendation to test all nursing home staff weekly would cost more than $1 billion every month.
“For months now, we have been advocating for expanded and priority testing in nursing homes to protect our residents and caregivers, but this is a significant undertaking and cost for nursing homes to shoulder on their own,” said Mark Parkinson, president and CEO of the AHCA/NCAL. “That’s why we have asked HHS to grant our request for a $10 billion emergency relief to help fund expedited testing and the additional staffing needed to respond to this unprecedented health crisis.”
New data from the nursing home trade group estimates COVID-19 testing at nursing home facilities nationwide will cost $440 million. In Arkansas, the cost for coronavirus testing at the nearly 28,000 nursing home residents and staff at the 126 log-term facilities across the state will exceed $4.2 million.