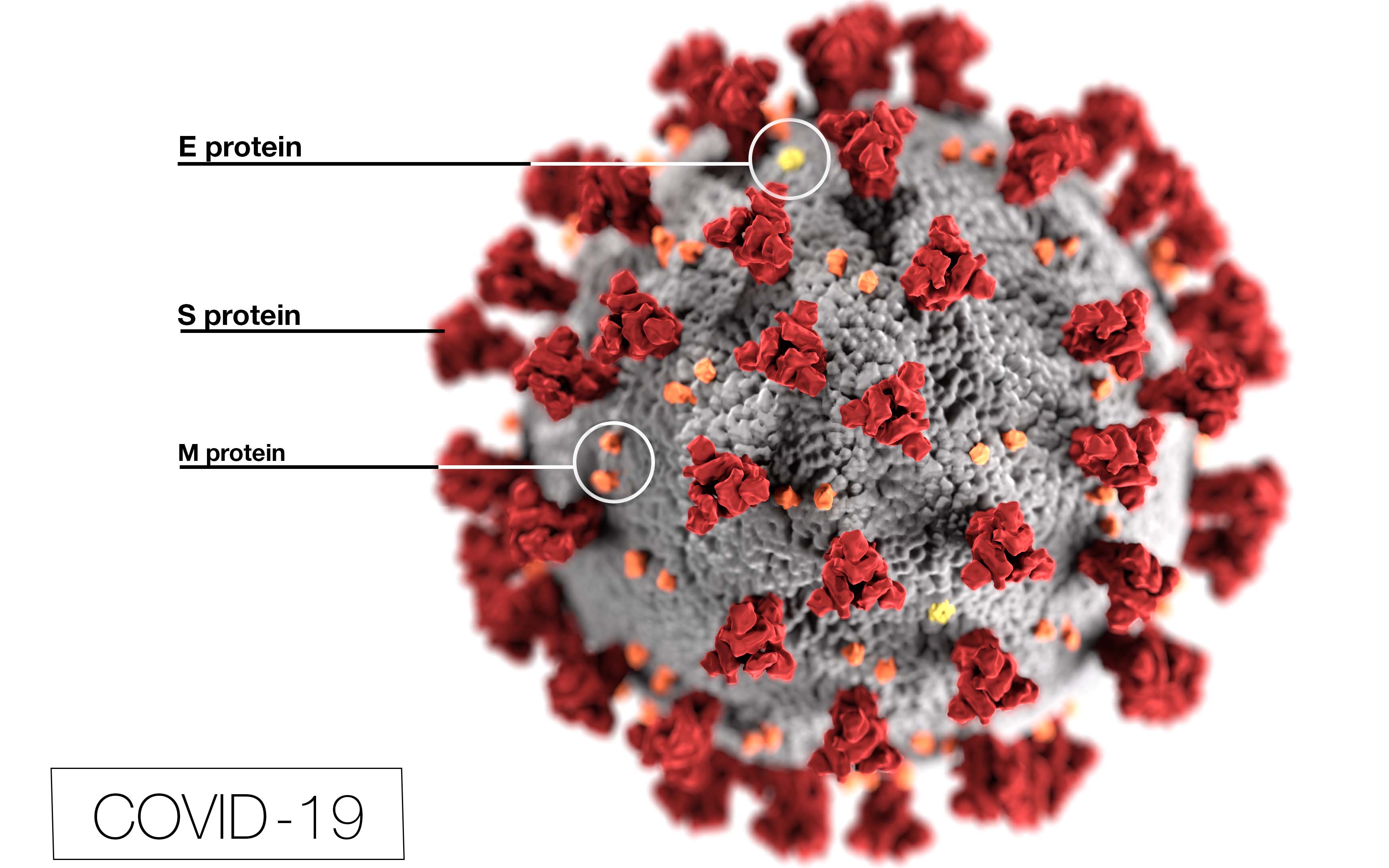
COVID-19 Small Business Resources
July 27 - August 2, 2020
Gov. Hutchinson issues executive order on mandatory face coverings in public
Faced with the continued spike in positive coronavirus cases across the state, Gov. Asa Hutchinson on July 18 issued an executive order calling for Arkansas residents to wear a face covering completely over their mouth and nose while in public.
The public directive, which excludes private homes, went into effect on July 20 and affects any indoor or outdoor public space where an Arkansas resident is exposed to non-household members and social distancing is not practical.
In line with recommendations from the U.S. Center for Disease and Control (CDC), the face mask must completely cover the mouth and nose or can be purchased commercially with an ASTM rating of at least Level 1, or homemade using at least two layers of material. The governor’s executive followed similar mandates in larger states and actions taken by Walmart, Kroger, Target, Amazon and other major retailers to stem the rise in the number of COVID-19 cases.
Hutchinson executive order, however, those exempt the following shall be exempt from wearing a face covering in Arkansas, including:
• Persons younger than 10 years of age (This requirement shall not supersede any decision by the Secretary of Education, public school district, or private school to require masks for children younger than 10 years of age while attending school);
• Persons with a medical condition or disability that prevents wearing a face covering;
• Persons performing job duties where a six feet distance is not achievable, but a mask is inhibitory to the ability to safely and effectively perform the job duty;
• Persons participating in athletic activities where a six feet distance is not achievable, but a mask is inhibitory to the activity or active exercise;
• Persons consuming food or drink;
• Persons driving alone or with passengers from the driver’s household;
• Persons receiving services that require access to the face for security, surveillance, or other purposes may temporarily remove a face covering while receiving those services;
• Persons voting, assisting voters, serving as poll watchers, or actively performing election administration duties; however, face coverings are strongly encouraged;
• Persons engaged in religious worship activities; however, face coverings are strongly encouraged; j. Persons giving a speech or performance for broadcast or to an audience; however, those persons shall safely distance from nearby individuals;
• Persons in counties where the Department of Health has certified that risk of community transmission of COVID-19 is low. To be considered low risk, the county must not have a newly identified case of COVID-19 for twenty-eight (28) consecutive days, assuming there has been adequate testing in the county.
NIH launches clinical trials network to test COVID-19 vaccines and other prevention tools
The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, has established a new clinical trials network that aims to enroll thousands of volunteers in large-scale clinical trials testing a variety of investigational vaccines and monoclonal antibodies intended to protect people from COVID-19.
The COVID-19 Prevention Trials Network (COVPN) was established by merging four existing NIAID-funded clinical trials networks: the HIV Vaccine Trials Network (HVTN), based in Seattle; the HIV Prevention Trials Network (HPTN), based in Durham, N.C.; the Infectious Diseases Clinical Research Consortium (IDCRC), based in Atlanta; and the AIDS Clinical Trials Group, based in Los Angeles. Those individual networks will continue to perform clinical trials for HIV vaccine and prevention and other infectious diseases in addition to their new COVID roles.
“Establishing a unified clinical trial network is a key element of President Trump’s Operation Warp Speed, which aims to deliver substantial quantities of a safe, effective vaccine by January 2021,” said HHS Secretary Alex Azar. “Starting this summer, this new network will leverage existing infrastructure and engage communities to secure the thousands of volunteers needed for late-stage clinical trials of promising vaccines.”
“Having a safe and effective medical countermeasure to prevent COVID-19 would enable us to not only save lives but also help end the global pandemic,” said NIAID Director Dr. Anthony Fauci. “Centralizing our clinical research efforts into a single trials network will expand the resources and expertise needed to efficiently identify safe and effective vaccines and other prevention strategies against COVID-19.”
The network’s vaccine testing will be led by Dr. Larry Corey, of the Fred Hutchinson Cancer Research Center in Seattle, and Dr. Kathleen M. Neuzil, of the University of Maryland School of Medicine. The network’s monoclonal antibody clinical testing efforts will be led by Dr. Myron Cohen, of the University of North Carolina, Chapel Hill, and David Stephens, M.D., Emory University in Atlanta. The HVTN, which is based at the Fred Hutchinson Cancer Research Center, will serve as the COVPN’s operational center.
The COVPN is a functional unit of “Operation Warp Speed,” a partnership led by the U.S. Department of Health and Human Services (HHS) to invest in and coordinate the development, manufacturing and distribution of COVID-19 diagnostics, therapeutics and vaccines. The network will use a harmonized vaccine protocol developed by the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) public-private partnership. This will enable analyses of correlates of protection across multiple vaccine trials. The network is expected to operate more than 100 clinical trial sites across the United States and internationally.
The network has developed an extensive community engagement framework to reach out to potential research volunteers and explain the specific details involved in participating in a vaccine or monoclonal antibody clinical study.
“Each of the Phase 3 clinical trials that the COVPN will conduct will require thousands of volunteers,” said NIH Director Dr. Francis Collins. “Community engagement, particularly with the communities most vulnerable to COVID-19’s severe outcomes, will be critical to the success of this research endeavor.”
People also can learn more about the different stages of vaccine research and the new network’s COVID-19 vaccine and monoclonal antibody studies by visiting the COVPN’s website (https://www.coronaviruspreventionnetwork.org(link is external)). The COVPN website features a customized data collection platform, which Oracle (Redwood Shores, CA) built and donated, to securely identify potential trial participants. Interested individuals can sign up for a rolling clinical trial participant registry on the website, which features security-enhanced protections. Clinical study staff will use the registry to contact and screen potential study volunteers.
The first Phase 3 clinical trial that the COVPN is expected to conduct will involve testing the investigational mRNA-1273 vaccine, developed by NIAID scientists and their collaborators at the biotechnology company Moderna Inc., based in Cambridge, Massachusetts. That study is expected to begin this summer.
Gilead Science provides additional data on antiviral remdesivir treatment of COVID-19
Gilead Sciences Inc., the first U.S. company to begin Phase 3 public trials for a COVID-19 vaccine, announced recently that the West Coast pharmaceutical has presented additional data on remdesivir, an investigational antiviral for the treatment of COVID-19.
The data were presented at the Virtual COVID-19 Conference on July 10 as part of the 23rd International AIDS Conference and included a comparative analysis of the Phase 3 SIMPLE-Severe trial and a real-world retrospective cohort of patients with severe COVID-19. In this analysis, remdesivir was associated with an improvement in clinical recovery and a 62 percent reduction in the risk of mortality compared with standard of care – an important finding that requires confirmation in prospective clinical trials.
Separate subgroup analyses from the Phase 3 SIMPLE-Severe trial, including an evaluation of the safety and efficacy of remdesivir across different racial and ethnic patient subgroups treated in the United States, found that traditionally marginalized racial or ethnic groups treated with remdesivir in this study experienced similar clinical outcomes as the overall patient population in the study.
Gilead is also presenting new analyses of the company’s compassionate use program, which demonstrated that 83% of pediatric patients and 92% of pregnant and postpartum women with a broad spectrum of disease severity recovered by Day 28. No new safety signals were identified with remdesivir across these populations. To further the understanding of these results in individual patient cases, Gilead recently announced the initiation of a global, open-label Phase 2/3 trial to evaluate the safety, tolerability and pharmacokinetics of remdesivir in pediatric patients from birth to less than 18 years of age. Gilead is also collaborating on a study for pregnant women.
Due to the current pandemic and public health emergency, the U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization for remdesivir for the treatment of hospitalized patients with severe COVID-19. However, remdesivir is an investigational drug that has not been approved by the FDA, and the safety and efficacy of remdesivir for the treatment of COVID-19 has not been established.
“We are working to broaden our understanding of the full utility of remdesivir. To address the urgency of the continuing pandemic, we are sharing data with the research community as quickly as possible with the goal of providing transparent and timely updates on new developments with remdesivir,” said Dr. Merdad Parsey, chief medical officer at the Foster City, Calif-based pharmaceutical giant. “These data presented at the Virtual COVID-19 Conference shed additional light on the use of remdesivir in specific patient populations, including those that may be susceptible to higher rates of COVID-19 infection, as well as others that are particularly vulnerable, including children and pregnant and postpartum women.”
In late June, Gilead first announced plans to start testing an inhaled version of remdesivir to determine whether it could treat COVID-19 sooner.` The Phase 3 SIMPLE-Severe trial evaluated the safety and efficacy of 5-day and 10-day dosing durations of remdesivir administered intravenously in hospitalized patients with severe manifestations of COVID-19.
The initial phase of the study randomized 397 patients in a 1:1 ratio to receive either a 5-day or a 10-day treatment course of remdesivir in addition to standard of care. The results were published in The New England Journal of Medicine in May. An expansion phase of the study was added to enroll up to 5,600 additional patients, including those on mechanical ventilation; results from the expansion phase are pending.