NIH begins study of allergic reactions to Moderna, Pfizer vaccines as total shots near 150 million
April 12-18, 2021
By Daily Record staff
As the total number of Americans that have received COVID-19 vaccinations nears 150 million, the Biden administration has launched a clinical trial to study allergic reactions to the Moderna or Pfizer-BioNTech COVID-19 vaccines.
Both Pfizer and Moderna in November first announced that their respective vaccines to received emergency authorization by the U.S. Food & Drug Administration (FDA) following successful COVID-19 Phase 3 investigational trails under the Trump administration’s Operation Warp Speed project. Subsequently, the FDA in December gave approval for both biopharmaceutical firms to begin manufacturing, distributing and administering their two-dose coronavirus vaccines in late 2020 and early 2021.
On Wednesday (April 7), President Joe Biden announced at a White House briefing that his administration was well on its way to hitting the goal 200 million shots by his 100th day in office. Biden, who was inaugurated as president on Jan. 20, encouraged Americans who have not received their COVID-19 shot to do. He also urged local and state government officials to keep U.S. Center for Disease & Control (CDC) mask mandates and social distance orders in place until the coronavirus is at bay.
“(Let) me be deadly earnest with you: We aren’t at the finish line. We still have a lot of work to do,” said Biden. “We’re still in a life-and-death race against this virus. Until we get more people vaccinated, we need everyone to wash their hands, socially distance, and mask up in a recommended mask from the CDC.”
While Biden was providing his COVID-19 vaccine update, the National Institute of Health (NIH) also announced the same day that a clinical trial is underway to determine whether people who are highly allergic. Those vaccine recipients who have a mast cell disorder are also at increased risk for an immediate, systemic allergic reaction to the Moderna or Pfizer-BioNTech vaccines, NIH officials said.
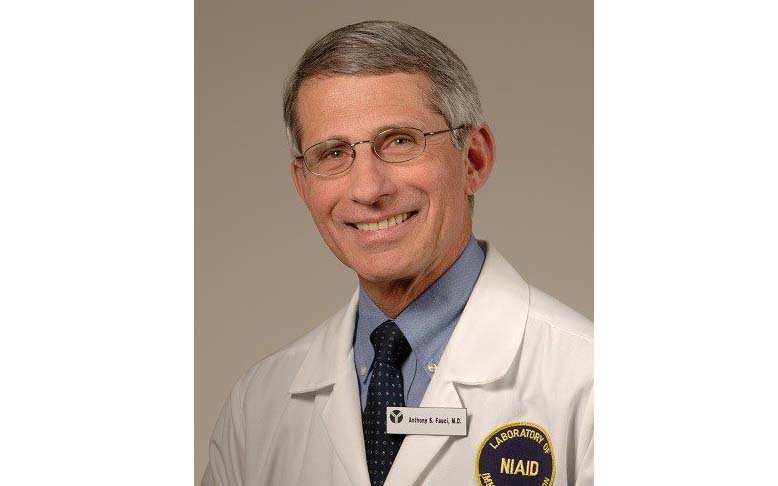
“The public understandably has been concerned about reports of rare, severe allergic reactions to the Moderna and Pfizer-BioNTech COVID-19 vaccines,” said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), part of the NIH. “The information gathered during this trial will help doctors advise people who are highly allergic or have a mast cell disorder about the risks and benefits of receiving these two vaccines. However, for most people, the benefits of COVID-19 vaccination far outweigh the risks.”
A systemic allergic reaction to a vaccine occurs in one or more parts of the body beyond the injection site, NIH officials said. If such an allergic reaction occurs in study participants, investigators will assess whether the reactions are more frequent in participants who are highly allergic or have a mast cell disorder than in participants with no allergic history. In addition, investigators will examine the biological mechanism behind the reactions and whether a genetic pattern or other factors can predict who is at most risk.
A mast cell disorder is a disease caused by a type of white blood cell called a mast cell that is abnormal, overly active, or both, predisposing a person to life-threatening reactions that look like allergic reactions. Since the COVID-19 vaccinations started shortly before Christmas, some Americans have been reluctant to get the coronavirus shot due to concerns over side effects and other notions about the vaccines, including some unverified conspiracy theories.
The Phase 2 trial, called Systemic Allergic Reactions to SARS-CoV-2 Vaccination, is sponsored and funded by NIAID. The vaccines are being provided by the program led by the U.S. Department of Health and Human Services and the U.S. Department of Defense to develop COVID-19 vaccines and therapeutics.
Although the Moderna and Pfizer-BioNTech COVID-19 vaccines were the first two COVID-19 vaccines authorized by the FDA for emergency use and already have been given to millions of Americans, most of the rare, severe allergic reactions to these vaccines have occurred in people with a history of allergies, NIH officials said. A substantial number of these people had previously experienced a life-threatening allergic reaction called anaphylaxis.
Women see higher COVID-19 allergic reactions, NIH says
The study team will enroll 3,400 adults ages 18 to 69 years at up to 35 academic allergy-research centers nationwide. About 60% of study participants, group 1, must have either a history of severe allergic reactions or a diagnosis of a mast cell disorder, while 40% of participants, group 2, will not. The specific types of allergic reactions in group 1 participants are related to food, insect stings or allergen immunotherapy and require treatment with a drug called epinephrine; or are immediate allergic reactions to a vaccine or to one or more drugs.
These reactions will have occurred within the past 5 years. Group 2 will consist of people with no history of any allergic reactions or allergic disease and no history of a mast cell disorder. Approximately two-thirds of participants in each group will be female, because severe allergic reactions to vaccines in general – and to the Moderna and Pfizer-BioNTech COVID-19 vaccines in particular – have occurred mainly in women.
Participants in each group will be assigned at random to receive either the Pfizer-BioNTech vaccine (one third of the group); the Moderna vaccine (one third); a placebo followed by the Pfizer-BioNTech vaccine (one sixth); or a placebo followed by the Moderna vaccine (one sixth). Initially, neither the participants nor the study team will know who is receiving a vaccine or placebo, or which vaccine is being administered. All participants ultimately will receive a full two-dose course of either the Pfizer-BioNTech vaccine or the Moderna vaccine.
The site investigators are allergists trained to recognize and treat anaphylaxis. Emergency medications, oxygen and medical equipment will be on hand to treat allergic reactions as needed. Participants will be observed for at least 90 minutes after each injection in case any type of reaction occurs.
Three days after their first injection, participants will receive a follow-up call from the study team to schedule their next injection in 21 or 28 days. Three days after the second injection, participants who did not receive a placebo will be told during a follow-up call that they received a vaccine and which one, while participants who initially received a placebo will be scheduled for their second dose of vaccine. Study staff will assess participants’ health during follow-up calls. All participants will receive their final follow-up call seven days after their last dose.
Investigators will assess the proportion of study participants in each group who have a systemic allergic reaction within 90 minutes after injection with either dose of the Pfizer-BioNTech vaccine or dose of the Moderna vaccine. Results are expected in late summer 2021.
Study staff will collect blood, urine and nasal swabs from participants before each injection, and blood and urine after each injection. If a significant number of systemic allergic reactions to either or both vaccines occur during the trial, investigators will analyze these biological samples to examine possible mechanisms for the reactions and whether certain genetic patterns are associated with higher risk.
Investigators will closely monitor participants’ safety throughout the trial. In addition, an independent data and safety monitoring board (DSMB) will review blinded and unblinded study data at scheduled review meetings to further ensure the safety of study participants.
The Systemic Allergic Reactions to SARS-CoV-2 Vaccination trial is co-chaired by Dr. N. Franklin Adkinson Jr., Dr. James R. Baker Jr., and Dr. Rebecca S. Gruchalla. Adkinson is a professor of medicine and director of the graduate training program in clinical investigation at the Johns Hopkins Asthma & Allergy Center in Baltimore. Baker is director of the Mary H. Weiser Food Allergy Center and is the Ruth Dow Doan Professor of Biologic Nanotechnology at Michigan Medicine in Ann Arbor. Gruchalla is a professor of internal medicine and pediatrics and chief of the divisions of allergy and immunology in the departments of internal medicine and pediatrics at the University of Texas Southwestern Medical Center at Dallas.
For more information about the trial, including a list of sites that are enrolling participants, go to ClinicalTrials.gov and search under study identifier NCT04761822.
PHOTO CAPTION:
(Covid variant) - Colorized scanning electron micrograph of a cell (orange) infected with UK B.1.1.7 variant SARS-CoV-2 virus particles (green), isolated from a patient. NIH.